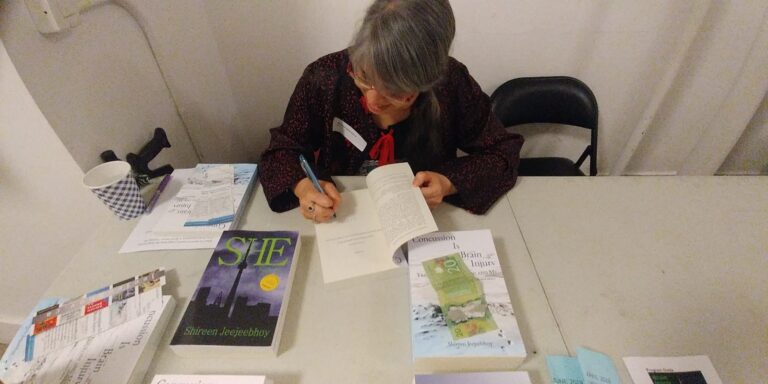
Reflecting on the past 25 years living with traumatic brain injury as I walk into the continuing fog of the future.
Category: Brain Health
Writings on brain injuries, remedies, and interesting tidbits, from the perspective of one who suffered a closed head injury and didn’t lose consciousness. Mild brain injuries are injuries too.
Blood Pressure Revisited
To figure out out what to do about my yo-yoing blood pressure, we have to look at my coping skills (fine), the actual stress I’m under (situational, emotional, physical, mental), my physical parameters (weight, diet, exercise), and how my brain has affected the whole shebang.
Health First
My guiding principle in brain injury recovery, heck life, is health above everything else. Without health, especially without treating the neurons, it’s virtually impossible to work, socialize, enjoy things. What strategies do you use to maintain your health and well-being? Following my principle of health first and setting myself up for success, I didn’t try…
Remembering, Believing Compassion In Tough Times
What quality do you value most in a friend? The title is the quality I value most. Until my brain injury, I believed I had friends who’d be there in sickness not just health. Until the Y2K car crash, I didn’t think about how important it is to remember the person that was before sickness…
You Would Not Want My Morning Ritual
What are your morning rituals? What does the first hour of your day look like? Oh wow. Talk about a question getting into the heart of life with brain injury, one that didn’t receive neuron-healing treatments for years and then only experimentally at first then one at a time over decades. And one with very…
The Tired Question
What is one question you hate to be asked? Explain. Tell me your story. It’s sort of a question wrapped up in a command. And, really, where would I begin‽ My story is so dang long! How about reading my memoir. Too long. My blog. Too many posts. Psychology Today blog. Where’s the post on…
My Life’s Opening Sentence
You’re writing your autobiography. What’s your opening sentence? I read mysteries. I live one, too. Brain injury is like a mystery. A grey and white thing hidden inside a roundish bony thing, the brain does its thing, running us and our bodies mysteriously until it is injured. None can see the damage. Not with their…
What Is My Job?
Do you enjoy your job? This Jetpack app prompt presupposes you have a job. Most people do, whether they think of it as a career or a way just to eat. I guess that means most are healthy enough — emphasis on enough — to work, to have enough stamina to keep working and earning.…
Watch to SmartWatch
I wore a watch since my 8th birthday until a few years after my brain injury when my skin and tolerance to skin irritation made me take it off. I figured I’d use TTC clocks (OK, hard to see after they upgraded to those screens), city clocks (where are they‽), or my Palm, later my…