We bought a Concept II rower back in the late 1990s, the same one athletes use for training. We both used it. Me with my blood pressure that had a tendency to drop under stress from lack of catecholamines, couldn’t do much in comparison to fit and tall him. But I was progressing up levels.…
Tag: Health care
Watch to SmartWatch
I wore a watch since my 8th birthday until a few years after my brain injury when my skin and tolerance to skin irritation made me take it off. I figured I’d use TTC clocks (OK, hard to see after they upgraded to those screens), city clocks (where are they‽), or my Palm, later my…
Medical Assistance in Dying, Bill C-7: A Letter To My MP on Euthanizing Disabled
Medical assistance in dying is suicide by another’s hand, one that was trained to heal and restore life. It’s now being targetted at people on the basis of disability. This issue is so serious the UN has weighed in on it. I wrote the following email to my MP this week (I’ve omitted my intro…
Meditech Rehabilitation Laser Centre
The Clinic Q&A Five is designed to help people discern what clinics will suit their brain injury needs best. Read what Meditech Rehabilitation Laser Centre will provide you in your recovery. I ask five questions; the clinic provides answers, links, images, video, and contact info. You get to compare and decide. This is a new feature,…
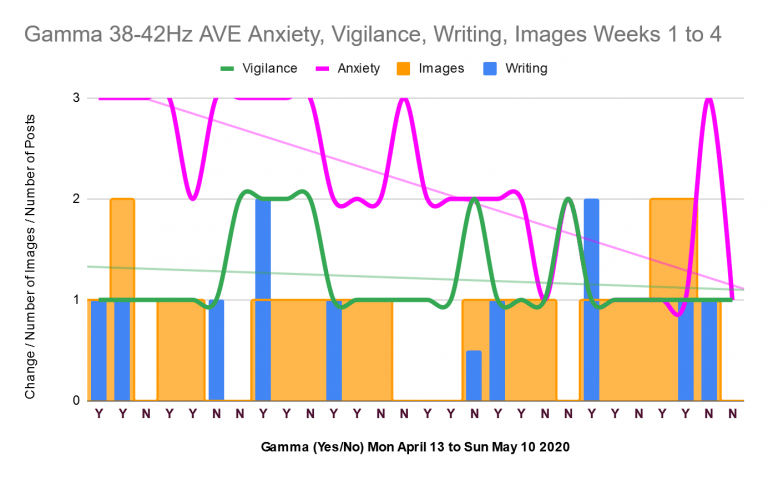
Gamma 38 to 42Hz Study: Results and Discussion
On 13 April 2020, I began a single subject study into audiovisual entrainment of gamma brainwaves at 38 to 42Hz. The ideal gamma brainwave frequency one wants is 40Hz. I finished it yesterday, 10 May 2020. Today, I present the results of four weeks of this study. Results I measured the effect of gamma 38…
Hope Malaise
My first blog was a political one. Hope in the form of writing fuelled it. I titled it “talk talk talk” because, despite my brain injury putting dampers on my thoughts and talking, I like to talk, debate, engage. Maybe that’s why my first followers thought I was male then most bailed once I outed…
Health Takes A Month
I’m being a dutiful and safe adult and getting my shots. I’ve had my pneumonia one, Prevnar 13, and the two Shingrix ones, for shingles. Next up is my tetanus booster, and I’m seriously wondering: do I hafta‽ I will get it, but I need a few weeks of my health back first. Brain injury…
Week One Lindamood-Bell Reading Comprehension Progress Report
All of a sudden, my first week at Lindamood-Bell Australia was done! Never so happy as to hear “we’ll stop there” as time was up in my second hour Thursday night. Yet vying with the fatigue was this alertness, this up state that my neurodoc described as excitement, excitement at starting something new and at…
Concussion Recovery is a Series of What are my Priorities?
As I come out of the narrow, tortuous pass that is a life focused on treating brain injury and the subsequent PTSD, I’m faced with the big question: what are my priorities? The first time I said bye to focusing on treating my injured neurons, I hunted for the supports I needed to be functional.…