The first part of this series is how I came to look at the hypothalamus. This post is more about general principles of how the hypothalamus works for those of us who aren’t physiologists, rather than a scientific treatise. However, I’ve included links for those who want to know the mind-bending details. I’d also like to note that knowledge of the hypothalamus is limited, contrary to the confident writing of many an author. As I noted in my article on reading, the brain is the final frontier.
The hypothalamus controls or runs the sympathetic nervous system (fight or flight) and the pituitary gland (the bane of adolescence), among other systems. In brain injury, most focus on the latter, if they do at all for internal functioning problems I’m discovering that many of us with brain injury have.
According to Medline Plus on the NIH (National Institutes of Health in the USA), the hypothalamus produces hormones that control or influence
- the pituitary and other hormonal glands to release their own hormones
- body temperature
- hunger
- thirst
- moods
- sex drive
- sleep
The hypothalamus is a small area of the brain below the larger thalamus (which controls it), just in front of and above the brain stem, and right above the pituitary stalk, which it controls.
As you can see from the above image, the tiny little hypothalamus controls much of your body’s functioning. Basically, the hypothalamus determines whether or not and how much each of those glands or body parts secretes their own hormones in order to keep your body in balance. Every one of those endocrine glands runs an important part of your functioning from sex to healing to rate of metabolism to stress response and affects your sense of well-being. For example, the hypothalamus may determine that you’re too hot; it’ll tell the thyroid to dial things down, and you will no longer feel hot but just right. The word used to describe this is homeostasis. This is where you want to be: in balance.
Scholarpedia has an extensive scientific article on the hormonal aspects of the hypothalamus, which you can read here. But the hypothalamus also controls your autonomic nervous system. This system controls the autonomic — automatic, if you will — part of your metabolism, like heart rate, blood pressure, breathing (though that is also under your conscious control), and emotional arousal. The autonomic nervous system comprises the sympathetic and parasympathetic nervous systems. The former puts you into the fight or flight response when stressed, through increasing the secretions of a hormone released by one-half of the adrenal glands called “adrenaline” or “epinephrine” via the hypothalamus and pituitary gland and of a neurochemical in the brain called “noradrenaline” or “norepinehprine.” When the stress is gone, the autonomic system will rebalance, decreasing the activity of the sympathetic system and increasing the parasympathetic system.
The hypothalamus receives information about how your body is functioning from several different sources. From the vagus nerve, it finds out how fast your heart is beating and how bloated your stomach is or not. From the reticular formation in the brain stem, it learns how hot or cold your skin is. From the optic nerve, which sends signals from the back of your eyeball, it finds out how light or dark it is where you are. From certain neurons in the spaces in your brain called “ventricles”, it finds out whether toxins are present, toxins that can lead to throwing up. From the rest of the limbic system and olfactory (your nose) system, it receives information that tells it your level of sexual arousal and whether you need to eat or not. It also has its own receptors, which measure ion balance and blood temperature. It’s a busy, busy brain part.
The hypothalamus is involved in the stress reaction in two ways: hormonally and through the sympathetic part of the autonomic nervous system. It takes in all the incoming information and decides if you are stressed. If it decides yes, it’ll decide if this gland or that one needs to secrete more of its hormones or less to deal with the stress and decides if it needs to activate the sympathetic system. When the incoming information tells it that the stress is gone, it’ll dial the sympathetic system down and rebalance it with the parasympathetic system, and it’ll send new instructions to the glands.
The sympathetic system is your fight or flight; the parasympathetic the homeostatic or normal state of good functioning. As a result, the hypothalamus affects heart rate, breathing, blood pressure, body temperature, water retention, emotional arousal, glucose metabolism, and so on. The chart below is what I drew to describe what happens when your hypothalamus activates your stress response and deactivates it.
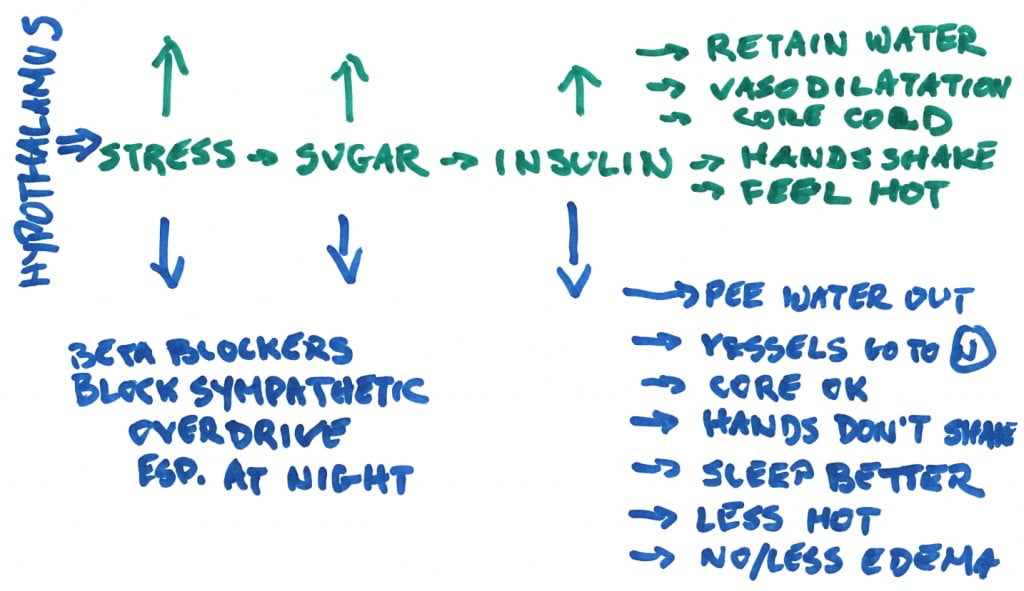 As you can see from this chart, the hypothalamus regulates the stress reaction. When stress increases, it releases glucose (sugar) from a compound called “glycogen” in your liver to provide the body with energy. The increase in blood sugar boosts insulin levels in the blood. Usually insulin facilitates the movement of glucose from the blood into muscles, but if you’re insulin resistant – meaning you resist this movement of glucose into muscle cells – then the glucose will go into fat cells instead. High insulin levels are associated with sodium retention if you’re insulin resistant. And all this results in higher body temperature; shaking hands; a cold core (your trunk) as blood is shunted from digestion to muscles; your blood vessels opening up in your skin or sometimes constricting (if you’re stressed due to fear like a bear attack), depending on the stress source; and water retention (the latter if insulin resistant). This prepares you to meet danger and decide if fighting or flying is the best course of action. Think that deer in the headlights that suddenly takes off.
As you can see from this chart, the hypothalamus regulates the stress reaction. When stress increases, it releases glucose (sugar) from a compound called “glycogen” in your liver to provide the body with energy. The increase in blood sugar boosts insulin levels in the blood. Usually insulin facilitates the movement of glucose from the blood into muscles, but if you’re insulin resistant – meaning you resist this movement of glucose into muscle cells – then the glucose will go into fat cells instead. High insulin levels are associated with sodium retention if you’re insulin resistant. And all this results in higher body temperature; shaking hands; a cold core (your trunk) as blood is shunted from digestion to muscles; your blood vessels opening up in your skin or sometimes constricting (if you’re stressed due to fear like a bear attack), depending on the stress source; and water retention (the latter if insulin resistant). This prepares you to meet danger and decide if fighting or flying is the best course of action. Think that deer in the headlights that suddenly takes off.
When the hypothalamus decides stress time is over, it reduces the reaction, drops blood sugar, drops insulin levels, and you become cooler, your hands stop shaking, your core warms up to normal, your blood vessels constrict or dilate back to normal, and you pee out the excess water you’d retained. Beta blockers like atenolol somehow act to block the sympathetic stress reaction so that you don’t retain water so much, your hands don’t shake, your core temperature remains normal, and so on. Or at least reduces these effects even if doesn’t normalize them.
At the same time the hypothalamus is activating the sympathetic system, it may also tell the pituitary to secrete a hormone to act on the other half of your adrenal glands, a teeny tiny organ near your kidneys. While one half of the adrenals secretes adrenaline (see above), the other half secretes cortisol. Cortisol is the most commonly known hormone involved in the stress reaction. When you think of how cortisol behaves, think steroids. That’s why severe stress reaction may make you bloat up with water retention like you’ve taken oral or injected steroids.
Chronic stress happens when this stress reaction through both the sympathetic system and cortisol doesn’t switch off. This constant state of “on” can cause increased blood sugars (think diabetes), increased cholesterol (which is needed for synthesis of cortisol), weight gain, depletion of minerals from the bones and can increase the chance of developing diabetes, heart disease, asthma, allergies, and autoimmune diseases.
Since the hypothalamus is so deep in the brain and far away from the rough interior of the skull, it’s thought it’s not damaged in closed head injury or traumatic brain injuries that don’t affect the deeper structures. But I think that assumption is wrong. Back in 1998, a group of American researchers at Mount Sinai Medical Center conducted a study to look at complaints of weight gain, body temperature, hair and skin changes, and so on. These kinds of changes have to do with the stress reaction (and other issues too). For example, in response to stress, hair falls out. But when the stress is over, it grows back in. Unfortunately, when your brain decides you need to be in permanent stress reaction mode, your hair does not grow back properly and continues to cycle in and out of loss. Although Mount Sinai did look into the prevalence of these symptoms, not much has been done with this information other than to study those in hospital with severe brain injuries. That does not help those of us living at home, suffering these unpleasant symptoms or those of us who had closed head injuries and were never hospitalized. Up here in Canada we’re worse off as these complaints remain ignored and unstudied.
There is more, much more to know about the hypothalamus, but the only other aspects I will mention are serotonin and emotions.
Serotonin is a neurotransmitter that has been implicated in depression. But it is more than that. Low serotonin not only results in depression but also decreases satiety (which would make you want to keep eating). Increasing serotonin can not only lift mood and increase satiety, but it will also drop body temperature. Other neurotransmitters and hormones can decrease body temperature, like peptides, dopamine, estrogen, norepinephrine, and opioid peptides.
As for emotions, that’s a complex subject. However, the anterior cingulate gyrus seems to be connected both to the prefrontal cortex for cognitive tasks and the hypothalamus for emotional control. And apparently is also associated with mental flexibility and shift changing – something that is diminished or absent in people with brain injuries. It has a direct connection to the heart, and the heart can thus influence the brain to increase the activity of the parasympathetic system. For example, deep breathing will change the heart rate variability to be in sync with the breath so that inhalation will increase variability and exhalation will decrease it. As the heart rate variability moves into sync with the breath, the parasympathetic system will increase to balance the sympathetic system. And you will become calm, less stressed.
However, it is difficult to deep breathe 24/7. Also, my point of view is that all the changes in me were caused by injury, that is a change in physiology including in the hypothalamus. These are not behaviour- or emotionally-induced changes. Thus I needed something that would act directly on my brain physiology to reset its functioning back to normal.
All this gave me enough information to decide that (a) the locus of my brain injury-induced problem was in the hypothalamus and not the pituitary gland and (b) I needed to increase serotonin levels in the hypothalamus. My main focus was dropping body temperature, water retention, and my skin’s propensity to develop hot spots. Any changes to heart rate, blood pressure, and shortness of breath would be a bonus. After discussions with mindalive.com, thinking about this (which I’ve been doing for years), I decided to try what I call my “hypothalamus fix.” That is the subject of my next post.
—————————–
Note: I didn’t think about emotional control when devising my “hypothalamus fix.” Although I knew that having my frontal lobes damaged meant less control over the primitive part of the brain, I did not understand the role the hypothalamus plays in brain injury anger or emotional instability. For years, my affect (emotions) were flat but every now and then would become intense and roller coaster before returning to flat. Since undergoing brain biofeedback, my affect has come closer to normal but I still had emotional instability, though not as intense. The question I am now asking is what role does the hypothalamus play in emotional control and in sudden on/off rage.
———————-
Part 1: The Hidden Secret of Brain Injury: Hypothalamus Dysfunction
Part 3: A Hypothalamus Fix for Closed Head Injury?
Part 4: A Hypothalamus Fix Followup
Part 5: A Hypothalamus Fix: Second Followup




